Glaucoma is a leading cause of irreversible
blindness worldwide. Intraocular pressure (IOP) is a monumental parameter in
the diagnosis and monitoring of glaucoma. Accurate measurement of IOP is the
hallmark for the management of glaucoma patients. IOP is the sole modifiable
risk factor; the reduction of which is known to slow the progression of this
potentially blinding condition.1-6
Goldmann Applanation tonometer (GAT) is
considered the ‘gold standard’ in IOP measurement being the most accurate and
reliable of all the tonometers invented so far. This
slit-lamp mounted device is based on the Imbert-Fick2, 7 principle,
which states that the pressure (P) inside an ideal, dry thin-walled sphere is
equal to the force (F) required to applanate its
surface, divided by the area (A) {3.06 mm} of flattening (P=F/A).
Air puff tonometers
(APT) are non-contact devices that applanate the
cornea by a puff of air and measure IOP by the time required to flatten a given
area of the cornea. Due to wide variations in readings, they are used largely
for screening purposes.7
Transpalpebral tonometers like Diaton have been developed recently and considered by some8,9 to be well-tolerated, portable, user-friendly,
light weight instruments that do not need topical anesthesia.
Whenever a new tonometer is developed, it is routine
practice to compare it to the existing, reliable tonometers.
No local studies have been performed on this transpalpebral
tonometer to compare it with other devices. Hence, we embarked on a study to
assess this transpalpebral tonometer, in terms of
practicality and accuracy of IOP measurements, and compared it with the precise
and renowned Goldmann tonometer; used routinely in
glaucoma patients, and with our air-puff tonometer used for routine screening
of every patient arriving at our out – patient department.
MATERIAL
AND METHODS
A total of 400 eyes of 200 random subjects
were included in this cross-sectional, comparative study carried out in the
last two weeks of November, 2013. The subjects included consenting presumably
normal adults attending our out-patient department, their attendants, hospital
staff and doctors volunteering for the study, 16 years of age and above (range
16-67).
Exclusion criteria included uncooperative
patients to any method of tonometry, previously known glaucomatous patients,
history of antiglaucoma drugs, trauma, ocular
disease, scarred corneas, or intraocular or refractive surgery, astigmatism2
of 3 diopters or more by autorefraction, diabetes or
other serious systemic ailments.
Air-puff Tonometry, followed by Diaton Tonometry, and lastly Applanation
Tonometry was performed in both eyes, to prevent applanation
induced lowering of IOP. The Air-puff tonometer that used was Canon Full Auto
Tonometer TX-F®. APT was done first by a single observer and a mean of three
readings was taken (Fig. 1).
Then transpalpebral
tonometry using the Diaton® tonometer (Fig. 2) was
done by two observers with comparable readings. This instrument is based on the
principle10 of determining the acceleration of a rod during free
fall, with a definite weight on interactive with the elastic eyeball through
the lids.The patient must be sitting in a chair with
the head in horizontal position, and the eyes gazing at the patient’s thumb
used for fixation at 45° angle. The observer should be at the side of the
patient. The tonometer must be vertical when switched on. The upper eyelid
should be manually retracted 1 mm above the limbus,
and three readings should be taken with the tonometer tip touching the lid
parallel to the lid margin, and the mean IOP is read on the scale (Fig. 3).
Lastly, applanation
tonometry was done by a single observer using the same Goldmann
Tonometer (Haag Streit AT 900®) (Fig. 4). The
instrument was calibrated according to the manufacturer’s instructions. The eye
was anaesthetized with Alcaine® (proparacaine
hydrochloride 0.5 %) eye drops (Alcon) and a fluorescein strip was placed in
the inferior conjunctival fornix to stain the tear
film. Three consecutive IOP readings were taken for each eye, with aseptic
precautions and the mean was calculated for each eye. All types of tonometry
were performed between 8:00 a.m. to 2:00 p.m. The difference in IOP readings
were compared between the three tonometers.
The data was collected on a performa noting the age, gender, and IOP measurements of
all three tonometers in a tabulated form.
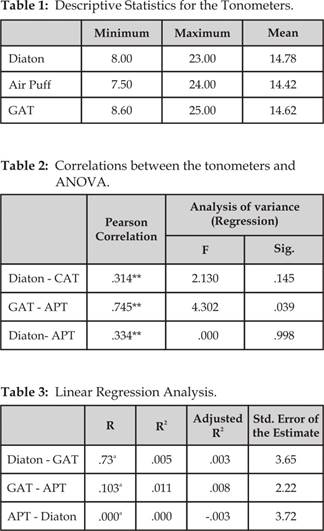
Data was analyzed by SPSS version 20. Mean IOPs and the
differences between IOPs of the tonometers were
calculated using the paired t-tests.
The correlations between the tonometers were
calculated using the Pearson correlation coefficients and the mean differences
between the tonometers was analyzed by one-way
analysis of variance. The agreement between the devices was analyzed by the
Bland-Altman method and plots were constructed between the means of IOPs (x axis), and the difference of IOPs (y axis), between the pairs of devices.
The mean IOP difference (bias) and the 95% limits of agreement; which represent
the range in which 95% of
Fig. 1: The Air Puff
Tonometer.

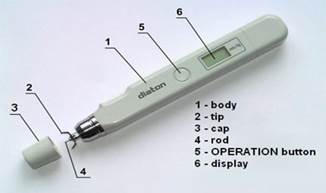
Fig. 2: The Diaton tonometer.
the differences between IOP measurements by the instruments
would occur; were analyzed for each pair. Linear regression analysis was
conducted on the IOP measurements of the three devices, and regression based
limits of agreement were analyzed.

Fig. 3: Procedure of Diaton tonometry.

Fig. 4: The Goldmann Applanation tonometer.
RESULTS
The average age of subjects enrolled in the study was
36.44 ± 13.76 years (range 16-67). There were 70 (35%) males and 130 (65%)
females. The mean IOPs noted for Diaton, GAT, and APT
were 14.78 ± 3.22 mm Hg
(range 8-23 mm Hg), 14.62 ± 3.01 mm Hg (range 8.6-25 mm Hg), and 14.42 ± 3.22
mm of Hg (range 7.5-24.4 mm Hg), respectively (Table 1). The difference of mean IOPs between GAT and Diaton was 0.16 ± 3.65 mm Hg, between Diaton
and APT was 0.36 ± 3.72 mm Hg, and between GAT and APT was 0.20 ± 2.23 mm
Hg. The mean Diaton
IOP was higher than GAT, while mean APT IOP was lower than GAT.
Diaton was seen to
overestimate IOP in 195 (48.8%) eyes, in comparison to Goldmann
IOP, underestimate IOP in 174 (43.5%), and gave equivalent IOP in 31 (7.8%)
eyes. The APT was found to be underestimating IOP in 204 (51%) eyes as compared
to GAT, overestimating in 179 (44.8%) eyes, and equal
IOP in 17 (4.3%) eyes.
The Pearson’s
correlation coefficient (r) between Diaton and GAT
was 0.314, between Diaton and APT was 0.334, and
between GAT and APT was 0.745 (Table 2). Hence, the strongest correlation was between GAT and
APT, followed by Diaton and APT, and least between Diaton and GAT. However, correlations between all three tonometers were significant at the 0.01 level.
Agreement between
the three devices was analyzed by the Bland-Altman analysis, which revealed the
mean difference (bias) between Diaton and GAT
measurements to be 0.16 ± 3.6 mm Hg (+7.33
to -7.01 mm Hg) (Fig. 5), and the mean difference between GAT and APT was 0.20 ± 2.2 mm
Hg (+ 4.57 to -4.17mm Hg) [Fig. 6], and
between Diaton and APT was 0.36 ± 3.7 mm Hg (+7.65 to -6.93mm Hg) (Fig. 7). This
shows good agreement between GAT and APT, and fair agreement of Diaton with both GAT and APT.
Linear regression analysis (Table 3)
was done which revealed R2 values between GAT and Diaton, GAT and APT, and APT and Diaton
to be 0.05, 0.01, and 0.00 respectively, indicating comparable performance
between the three. Analysis of variance between the three tonometers,
showed that GAT and APT could be used interchangeably (p=0.03) (Table 2).
DISCUSSION
Accuracy of IOP
measurement is the need for doctors managing glaucoma patients. Goldmann Applanation tonometer
has surpassed all other tonometers in terms of
reliability, accuracy, and is the benchmark of IOP measurement. It is precise,
easy to use with the slit lamp, and has low intra- and inter-observer
variability11. However, the effect of central corneal thickness,
astigmatism, and corneal curvature, on influencing IOP measurements with GAT,
is well-known.2,7,12-15A thick central
cornea leads to overestimating of the IOP, and vice versa. The IOP is
underestimated for with-the-rule astigmatism and overestimated for
against-the-rule astigmatism.16 Tonometers
that have been developed over the years have often been compared to this
indisputable tonometer.
Our study shows
that IOPs measured with GATand APT have good
correlation, while both APT and Diaton, and GAT and Diaton have moderate correlations; with the least
correlation was found between GAT and Diaton. Amongst
the three devices, good agreement was seen between GAT and APT, and
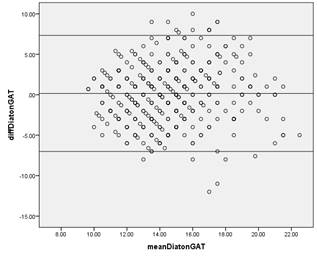
Fig. 5: Agreement between GAT and Diaton
(Bland-Altman plot).
Difference between Goldmann Applanation Tonometer
(GAT) and Diaton transpalpebral
tonometer plotted against mean IOP. The middle line indicates the estimated
mean GAT- Diaton difference. The upper and lower
lines represent the 95% limits of agreement for the difference (+7.33 to -7.01
mm Hg).
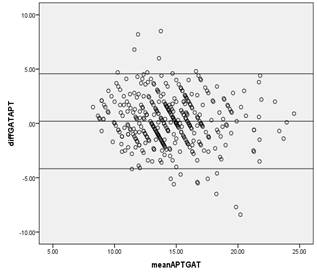
Fig. 6: Agreement between GAT and APT (Bland-Altman
plot).
Difference between Goldmann Applanation Tonometer
(GAT) and Air Puff tonometer (APT) plotted against mean IOP. The middle line
indicates the estimated mean GAT-APT difference. The upper and lower lines
represent the 95% limits of agreement for the difference (+4.57 to -4.17mm Hg).
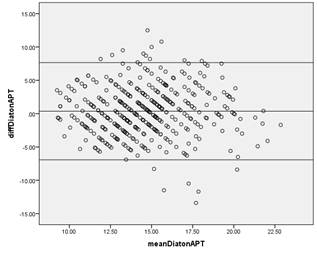
Fig. 7: Agreement between Diaton
and APT (Bland - Altman plot).
Difference between Diaton and Air Puff tonometer (APT) plotted against mean
IOP. The middle line indicates the estimated mean Diaton
- APT difference. The upper and lower lines represent the 95% limits of
agreement for the difference (+7.65 to -6.93mm Hg).
there was fair
agreement of Diaton with both GAT and APT.
Studies carried
out by Doherty,8 Bali,17 Li18
and Lösch19 et al, showed that Diaton and
other transpalpebral tonometer measurements did not
correlate much with GAT, and the two devices had poor agreement. The mean IOP
difference was 1.62 ± 3.60 mm Hg in the study by Li,18
and in numerous other studies, the limits of agreement were found to be very
wide, + 8.4 to – 9.6 observed by Doherty8 et al, + 4.4 to -11.8 seen
by Losch19, and -9.9 to + 11.2 in Bali’s study.17
Similarly, studies19 carried out by Troost20 et al
revealed transpalpebral tonometry to significantly
underestimate IOP compared to GAT, with the effect being more pronounced as the
IOP rises. This contrasts with our study, in which Diaton
overestimated IOP in the majority of eyes. Sandner21 and Toker22
et al have showed moderate correlation between GAT and lid tonometry, with a
wide variation21 in IOP noted with the latter. We too noted the wide
variation in IOP measured by Diaton. The above, in
their experience recommend lid tonometry as a screening tool or, in cases where
GAT is not possible like scarred corneas. However, we would not recommend usage
of Diaton in routine clinical practice and do not
consider it to be a useful device.
Numerous studies
have been carried out comparing the Air-puff tonometers
with GAT. A study carried out in Bahawalpur23 listed the accuracy of
APT as 49.7% with greater accuracy in the lower IOP range, when compared to
GAT. Similarly, a study conducted in North India24 shows a fair
agreement between APT and GAT when the IOP is in the lower range (mean IOP 1.2
mm Hg with limits of agreement +4.7 to –2.3), but a high correlation, similar
to our study. Here too, the air puff was found to under-estimate IOP in the
majority of cases, like we noted in our study. Salim25 et al in
their study in USA found a mean difference of -0.3 with limits of agreement of
+6.8 to -7.4, and Parker26 et al in UK noted mean IOP of –0.11 mm Hg
(limits +2.10 to –2.33)thus revealing comparable
performance of APT with GAT, with good agreement in the normal IOP range;
however the variation began with higher IOP range. On the contrary, a study
carried out in Iraq by Farhood27 et al, found significant
differences between the two devices, with APT overestimating IOP in as many as
74% cases with a mean difference of 2.72 ± 2.34 mm Hg.
A major limitation
of our study is that we have carried out the study on presumably normal
subjects because we wanted to compare IOP measurement by the three devices, in
the normal range of IOP. A few subjects with high IOPs were eventually
diagnosed as glaucomatous later on. This prevents us from comparing the devices
in the higher range of IOPs. Because of the smaller sample size, we were unable
to assess the above. We believe a larger scale study would be needed to assess
the devices in extremes of IOP. Another limitation is our lack to assess the
central corneal thickness of our subjects, and to evaluate its effect on the
three individual devices. We plan to investigate the above at a later stage, in
a separate study.
Some may consider transpalpebral
tonometry to be useful for screening purposes, because it is portable, user
friendly, and non-contact, but we do not deem it very useful in our practice,
due tovariability of IOP, difficult positioning of
the patient, and wide variation in measurement. Also, the slit-lamp mounted applanation tonometer is far more useful, accurate and
convenient for us to use. The air-puff tonometer has been used and recommended
largely for screening of patients, and has good agreement with GAT, so we
consider it to be a useful tonometer in our out-patient department for
screening of every patient presenting to us. However, we do confirm the IOP by
GAT in cases of glaucoma and when suspicion may arise.
CONCLUSION
Compared to Goldmann tonometry,
both air-puff tonometer and Diaton have good
correlation; however, only APT has good agreement with GAT, while Diaton has fair agreement with the two devices. APT is a
useful tool for screening of IOP, but Diaton cannot
be recommended as an accurate screening tool, due to wider variations in IOP.
Author’s Affiliation
Dr. Sana Nadeem
Assistant Professor
Department of Ophthalmology
Foundation
University Medical College /
Fauji Foundation Hospital, Rawalpindi
Dr. B.A. Naeem
Professor and Head Department of
Ophthalmology,
Foundation
University Medical College/
Fauji Foundation Hospital, Rawalpindi
Dr. Rabeea Tahira
Postgraduate Trainee, Department of
Ophthalmology
Foundation
University Medical College/
Fauji Foundation Hospital, Rawalpindi
Dr. Shizza Khalid
House Surgeon, Department of Ophthalmology
Foundation
University Medical College/
Fauji Foundation Hospital, Rawalpindi
Dr. Abdul Hannan
Post-graduate trainee
Al-Shifa Trust Eye
Hospital, Rawalpindi
REFERENCES
1.
Leske MC, Heijl A, Hussein
M, Bengtsson B, Hyman
L, Komaroff E. Early Manifest Glaucoma Trial Group. Factors for glaucoma progression and
the effect of treatment:
the early manifest glaucoma trial. Arch Ophthalmol.2003; 121: 48-56.
2.
Jerome C, Ramos-
Esteban, Katz LJ, Goldberg W, Goldberg A. Glaucoma.
Evaluation and Diagnosis. Clinical examination of glaucoma. In: Yanoff M, Duker JS.
Ophthalmology. Third Edition. Mosby: Elsevier. 2009; 1117-27.
3.
Gordon MO, Kass MA. The Ocular Hypertension Treatment
Study: designand baseline description
of the participants. Arch Ophthalmol.1999; 117: 573-83.
4.
Weinreb RN, Aung T, Medeiros FA. The pathophy-siology
and treatment of glaucoma: a review. JAMA.2014; 311: 1901-11.
5.
The effectiveness of intraocular
pressure reduction in the treatment of normal –
tension glaucoma. Collaborative Normal – Tension Glaucoma
Study Group. Am J Ophthalmol.1998; 126: 498-505.[
6.
Heijl A, Leske MC, Bengtsson B, Hyman
L, Bengtsson B, Hussein
M. Early Manifest
Glaucoma Trial Group. Reduction of
intraocular pressure and glaucoma progression: results from
the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002; 120: 1268-79.
7.
Cioffi GA, Durcan FJ, Girkin CA, Gupta N, Piltz-Seymour
JR, Samuelson TW, Tanna AP, Barton K, O’Connell SS. Glaucoma. Section
10. Basic and Clinical Science Course. AmericanAcademy
of Ophthalmology. San Francisco. 2012; 22-6.
8.
Doherty
MD, Carrim ZI, O'Neill
DP. Diatontonometry: an assessment of
validity and preference against Goldmann tonometry. Clin Experiment Ophthalmol. 2012; 40: 171-5.
9.
Waisbourd M, Shemesh G, Top LB, Lazar M,
Loewenstein A. Comparison of the
transpalpebral tonometer TGDc-01 with Goldmann Applanation tonometry. Eur J Ophthalmol. 2010; 20:
902-6.
10.
Troost A, Yun SH, Specht K, Krummenauer F, Schwenn O. Transpalpebral tonometry:
reliability and comparison with Goldmann applanation tonometry and palpation in healthy volunteers. Br J Ophthalmol. 2005; 89: 280–3.
11.
Dielemans I, Vingerling JR, Hofman A,Grobbee DE, de
Jong PT. Reliability of
intraocular pressure measurement with the Goldmann applanation tonometer in epidemiological
studies. Graefes Arch Clin Exp Ophthalmol. 1994; 232: 141-4.
12.
Mark
HH, Mark
TL. Corneal astigmatism
in applanation tonometry.
Eye, 2003; 17: 617-8.
13.
Rask
G, Behndig A. Effects of corneal thickness,
curvature, astigmatism and direction of gaze on Goldmann applanation tonometry readings.
Ophthalmic Res. 2006; 38: 49-55.
14.
Whitacre MM, Stein
RA, Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993; 115: 592-6.
15.
Lleó A, Marcos
A, Calatayud M, Alonso
L, Rahhal SM, Sanchis – Gimeno JA. The relationship
between central corneal thickness and Goldmann applanation tonometry. Clin Exp Optom. 2003; 86: 104-8.
16.
Akram A, Yaqub A, Dar AJ, Fiaz. Pitfalls in Intraocular Pressure
Measurement by Goldmann – Type Applanation
Tonometers. Pak J Ophthalmol.
2009; 25: 22-4.
17.
Bali SJ, Bhartiya S, Sobti A, Dada T,
Panda A. Comparative evaluation of Diaton and Goldmann applanation tonometers. Ophthalmologica. 2012; 228: 42-6.
18.
Li Y, Shi J, Duan X, Fan F. Transpalpebral
measurement of intraocular pressure using the Diaton
tonometer versus standard Goldmann applanation tonometry. Graefes
Arch Clin Exp Ophthalmol. 2010; 248: 1765-70.
19.
Lösch A, Scheuerle A, Rupp V, Auffarth G, Becker M. Transpalpebral measurement of
intraocular pressure using the TGDc-01 tonometer versus standard Goldmann applanation tonometry. Graefes Arch Clin Exp Ophthalmol. 2005; 243: 313-6.
20.
Troost A, Specht K, Krummenauer F, Yun SH, Schwenn O.
Deviations between transpalpebral
tonometry using TGDc-01 and Goldmann applanation tonometry depending on the IOP level. Graefes Arch Clin Exp Ophthalmol. 2005; 243: 853-8.
21.
Sandner D, Böhm A, Kostov
S, Pillunat L. Measurement of
the intraocular pressure with the “transpalpebral
tonometer” TGDc-01in comparison with applanation
tonometry. Graefes Arch Clin
Exp Ophthalmol. 2005; 243:
563-9.
22.
Toker MI, Vural A, Erdogan H, Topalkara A, Arici MK. Central corneal thickness and Diaton transpalpebral tonometry. Graefes Arch Clin Exp Ophthalmol. 2008; 246: 881-9.
23.
Ahmad J, Khan MR, Azhar
MN, Arain TM, Qazi ZA. Accuracy of IOP
Measured By Non-Contact (Air – Puff) Tonometer Compared with Goldmann Applanation Tonometer.
Pak J Ophthalmol. 2014; 30: 20-3.
24.
Mohan S, Tiwari S,
Jain A, Gupta J, Sachan SK. Clinical comparison of Pulsair
non-contact tonometer and Goldmann applanation tonometer in Indian population. Journal of
Optometry. 2014; 7: 86-90.
25.
Salim S, Lin DJ, Echols II JR, Netland
PA. Comparison of intraocular pressure measurements with the
portable PT100 noncontact tonometer and Goldmann applanation tonometry. Clinical Ophthalmology 2009; 3:
341–4.
26.
Parker VA, Herrtage J, Sarkies NJC. Clinical
comparison of the Keeler Pulsair 3000 with Goldmann applanation tonometry. Br J Ophthalmol. 2001; 85: 1303–4.
27.
Farhood QK. Comparative evaluation of intraocular pressure with an
air–puff tonometer versus a Goldmann applanation tonometer. Clinical Ophthalmology. 2013; 7:
23–7.